
Using advanced genetic mapping to potentially unlock groundbreaking new ependymoma treatments
Thanks to the ongoing generosity of our donors, we are bringing new hope to high-risk childhood ependymoma patients. Our organization is beyond excited to partner with Dr. Nicholas Foreman (one of our longest standing esteemed physician scientists) and his team at The Morgan Adams Foundation Pediatric Brain Tumor Research Program to bring to fruition an incredibly promising study focused on a particularly challenging high-risk pediatric brain cancer – ependymoma.
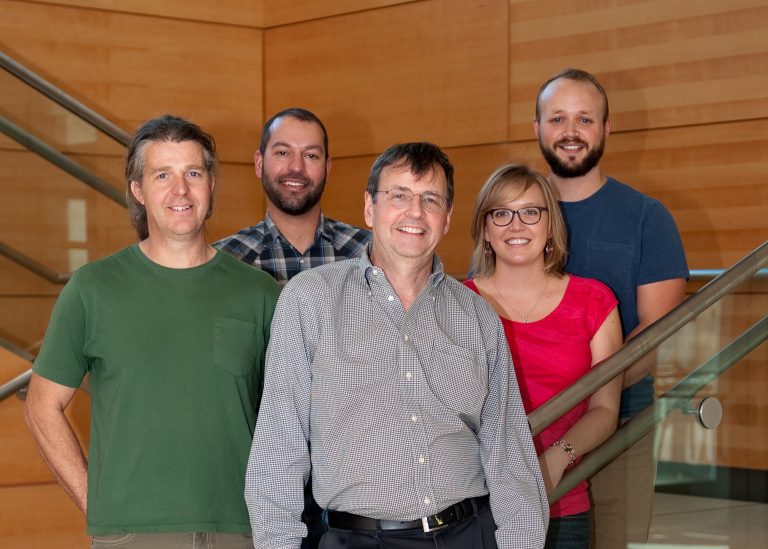
Through our partnership, Dr. Foreman and team have been investigating the better outcomes achieved when targeting a specific chromosome (chromosome 1q) known to cause the onset of ependymoma tumor growth as well as its recurrence.
Their team has now gone one step further – identifying the very genes on this chromosome that are the key triggers for the tumor cell development. This has enabled them to potentially target these trigger genes’ weaknesses – and develop new advancements that could make existing treatments exponentially more effective.
A clinical trial for two drugs that target these trigger genes in currently already underway. If successful, the results could lay the groundwork for an entire new generation of targeted therapies for high-risk ependymoma patients!
Want to learn more about the science behind this and other studies you’re helping to fund?
What is pediatric ependymoma?
Ependymoma is a type of brain tumor that typically affects children under 5. It arises from abnormalities in the cells lining the brain and spinal cord ventricles. Ependymoma can occur anywhere in the central nervous system, but in children, tumors are most common in the posterior fossa, which is the back of the brain.
Ependymoma is the third most common childhood brain tumor. Current treatment for ependymoma includes surgical removal of the tumor and radiation. More than 70% of kids treated for ependymoma relapse within 10 years and there are very limited options for those children who relapse.
Ependymoma, particularly the posterior fossa group A (PFA) subtype, remains one of the most challenging pediatric brain tumors to treat due to its aggressive nature and poor outcomes.
When a cancer patient survives five years from the end of treatment, most medical teams consider it a success. However, for some pediatric brain cancers like ependymoma, being disease-free at five years does not equal a cure.

Learning more about the lives you’re supporting
Meet Abbie, diagnosed with Ependymoma at 11
In October 2019, ten-year-old Abbie began throwing up after she woke up in the morning. Over the course of the next nine months and many doctor’s visits, a change in diet and supplements helped her feel better. But in July 2020 shortly after her 11th birthday, Abbie woke up with a migraine and she started seeing double.
Abbie went in for an eye exam and her mom explained to the optometrist what had been going on. When the optometrist looked at Abbie’s eyes, she noticed something that prompted some additional tests. The doctor determined that Abbie’s optic nerves were severely swollen and she would consult with an ophthalmologist.
Within an hour of leaving, the ophthalmologist called and told Abbie’s mom that he had ordered an emergency MRI for Abbie the next morning. A few hours after the MRI, the ophthalmologist called because Abbie had a large mass in the back of her head and she needed to get to Children’s Hospital Colorado right away.
At Children’s Colorado, Abbie had another MRI the next morning to check her spine, which was clear. Abbie underwent a 10-hour surgery to remove the tumor a few days later on August 3rd. Abbie started physical, occupational, and speech therapy and was discharged ahead of schedule. At the follow-up appointment, Abbie and her parents learned she had a posterior fossa group B ependymoma, a rare pediatric brain tumor. Abbie’s primary oncologist consulted with Dr. Nick Foreman to determine her treatment and she began 33 days of radiation in September and October. She then received three rounds of intense chemotherapy from December 2020 through February 2021.
Following treatment, Abbie went for scans every three months. When she got to a year post-treatment, her scans moved to every six months. In March 2024, her doctor said she is doing so well that she can do scans once a year.
Today, Abbie is 15 years old and enjoying life as a regular teenager. She is excited to get her driver’s permit and celebrate her Sweet Sixteen this summer. Abbie’s treatment was driven by the work done by Dr. Foreman and his research team, and her family is grateful to everyone who helped make it possible.

Want to learn more about the science behind this and other studies you’re helping to fund?